Partnership HealthPlan of California (PHC) has developed a 340B Compliance Program with the direction from the PHC 340B Advisory Committee.
Background - 340B Drug Purchasing Program
340B is the Section of the Public Health Services Act that allows certain eligible health care entities (Covered Entities) to get discounted drugs. The 340B Drug Purchasing Program was intended to "enable [participating] entities to stretch scarce Federal resources as far as possible, reaching more eligible patients and providing more comprehensive services." This includes Federally Qualified Health Centers, Rural Health Centers affiliated with Critical Access Hospitals, Family Planning Clinics, Indian Health Centers, and several classes of hospitals.
340B Requirements
At its core, federal law around 340B requires that 340B medications not be subject to duplicate discounts. That means if a drug is purchased at the 340B price, a State Medicaid Agency cannot claim a rebate on that same medication (42 USC 256b(a)(5)(A)(i)). 340B Covered entities must have mechanisms in place to prevent duplicate discounts. In states where Managed Care Plans are used, the Managed Care Plan is an agent of the State, meaning the Managed Care Plan is responsible for ensuring compliance with this requirement under Section 340B of the Public Health Services Act.
PHC's 340B Compliance Program
Overview:
PHC has developed a 340B Compliance Program to help bring the Plan and its 340B Covered Entity partners who have billed and will bill PHC for 340B drugs into compliance with the requirements of the 340B Drug Pricing Program. The 340B Compliance Program requires compliant claiming of all 340B drug billing for drugs dispensed to PHC members at Contract and In-House Pharmacies or as Physician-Administered Drugs (PADs).
Reclassification of 340B Drug Claims:
- 340B Reclassification of Medical/PAD claim service lines requiring the addition of the UD modifier
To request the addition of a UD modifier to a previously paid claim service line(s), please contact the PHC Pharmacy Department via email at 340BQIP@partnershiphp.org.
Please refer to the second attachment of the 340B Compliance Program Policy (see above) for complete instructions on this process.
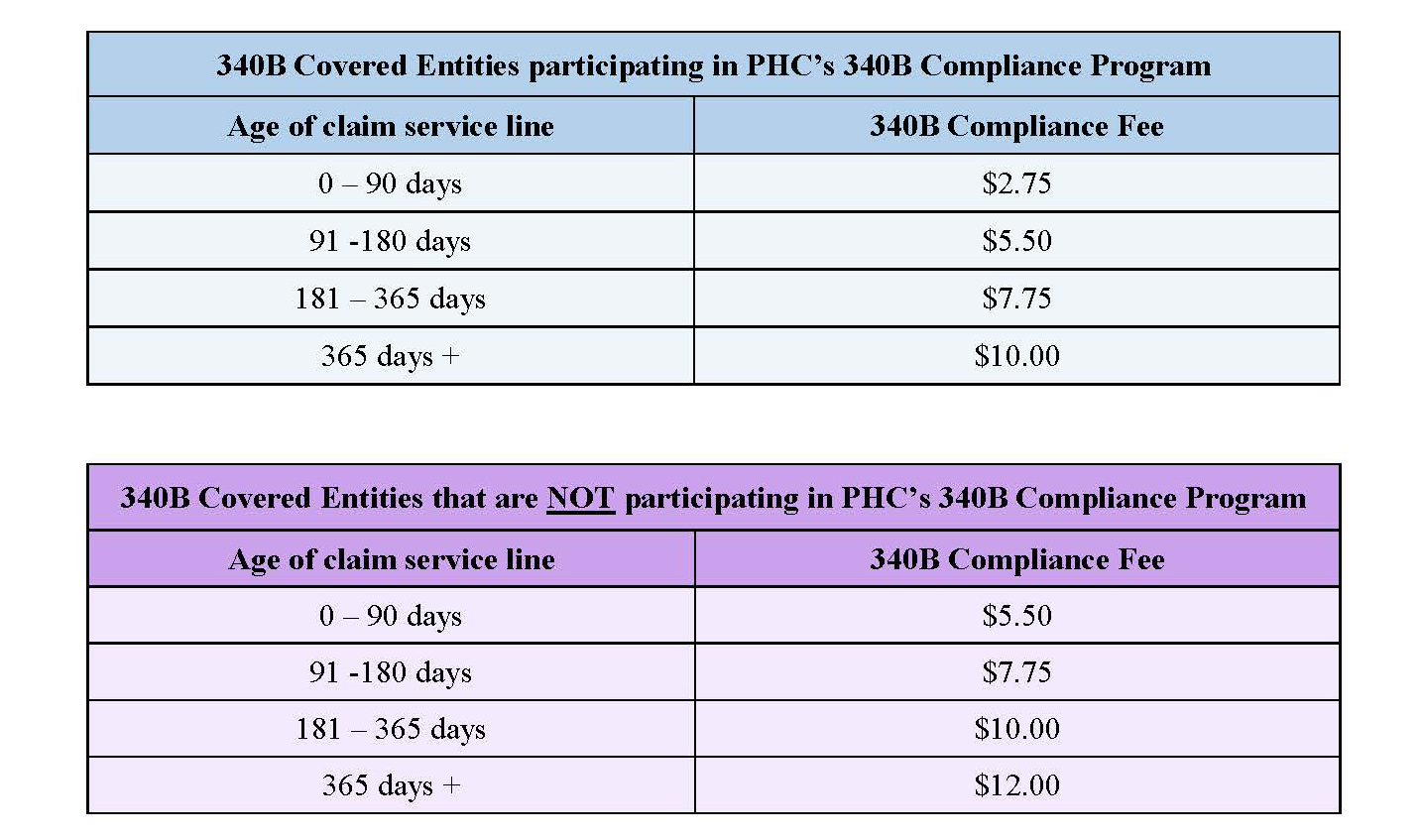
Please note that there will be 340B Compliance Fees assessed for this service based on the number of adjusted claim service lines and the dates of service involved.
- 340B Reclassification of Contract and In-House Pharmacy Claims
- Please refer to the 340B Compliance Program Policy and 340B Compliance Program Agreement for complete details and instructions on this process.
- 340B Covered Entities must participate in PHC's 340B Compliance Program in order to access services to reclassify Contract Pharmacy 340B claims and In-House Pharmacy 340B claims processed by PHC's Pharmacy Benefits Manager (PBM), MedImpact.